When the Medical Industry Manages Birth in Arkansas...
Who are we leaving out of this discussion?
I am tickled that Dr. Manning of UAMS on the Arkansas Maternal Mortality Review Committee keeps talking about midwifery and doulas as a solution to the crisis in women’s health here in Arkansas.
There is a serious disconnect between what is happening and what needs to happen, and it is very difficult to see the solution when you have been trained your whole career in what is good medical practice, and what our culture has come to expect as good health care for women.
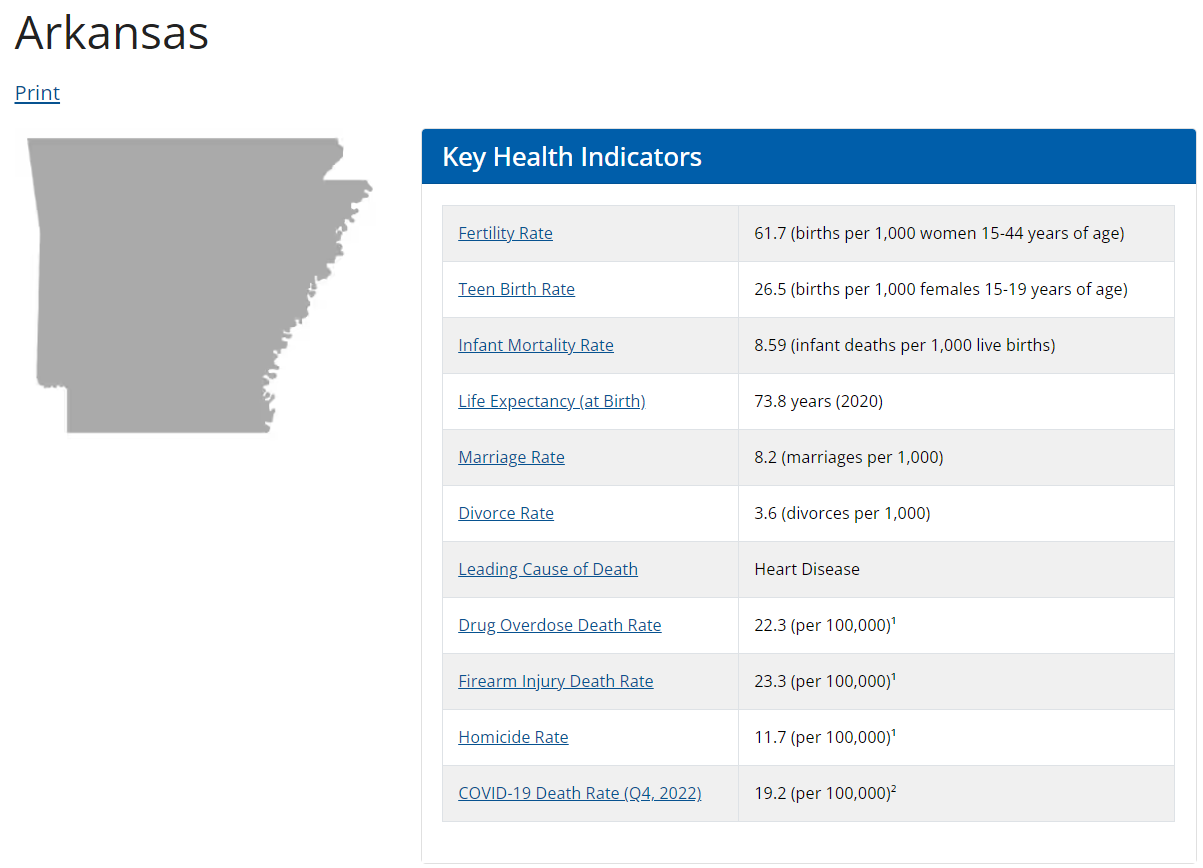
This week in the Arkansas Democrat-Gazette they announced $500,000 to be allocated to get a Certified Nurse Midwifery (CNM) school in Arkansas. There are two problems with this proposition. Let me preface this with support for the CNM community and that yes, we need more CNMs in birthing hospitals—absolutely. But that money came to the midwifery school at the expense of the Arkansas Center for Health Improvement (ACHI) whose mission is: “to be a catalyst for improving the health of Arkansans through evidence-based research, public issue advocacy, and collaborative program development.” They measure health outcomes in the state. We need this. We can’t afford to implement new measures at the expense of our data collectors who tell us when we are having issues and with what. The second issue with this CNM school is that the medical model for birth in Arkansas does not work and does not even exist in rural areas of Arkansas. We need to direct energy to the people who have not been invited to these discussions—Licensed Lay Midwives (LLMs).
I want to pause here and define terms.
Doula = This is a support person and advocate for a birthing mother. The doula provides encouragement and reassurance as well as advocating for the birthing mother in whatever setting the birth is taking place, but especially in a hospital environment.
Licensed Lay Midwife (LLM) = a designation only found in Arkansas, no other state. These are midwives who have been to midwifery school, apprenticed, and are licensed in Arkansas to provide professional midwifery care. According to the LLMs I have talked to in the state, they would like to change the designation in Arkansas to Certified Professional Midwives and do away with the “Lay” designation. LLMs practice mostly in home births, birth centers, and can follow a transferred patient into the hospital setting if allowed by the receiving hospital.
Certified Professional Midwife (CPM) = As of this writing there are 31 LLMs in Arkansas. 29 of them hold the title of Certified Professional Midwife. This is a national certification. The LLMs who do not also have CPM certification in Arkansas have been grandmothered in with their qualifications and have the required experience to practice in the state of Arkansas. These midwives practice mostly in home births, birth centers, and can follow a transferred patient into the hospital setting if allowed by the receiving hospital.
Certified Nurse Midwife (CNM) = This is a Registered Nurse who has gone on to get a master’s degree in Nurse Midwifery. While they do not have to practice exclusively in a hospital setting, that is where they are more commonly seen. It is my understanding that there are currently 2 CNMs who provide home births in Arkansas.
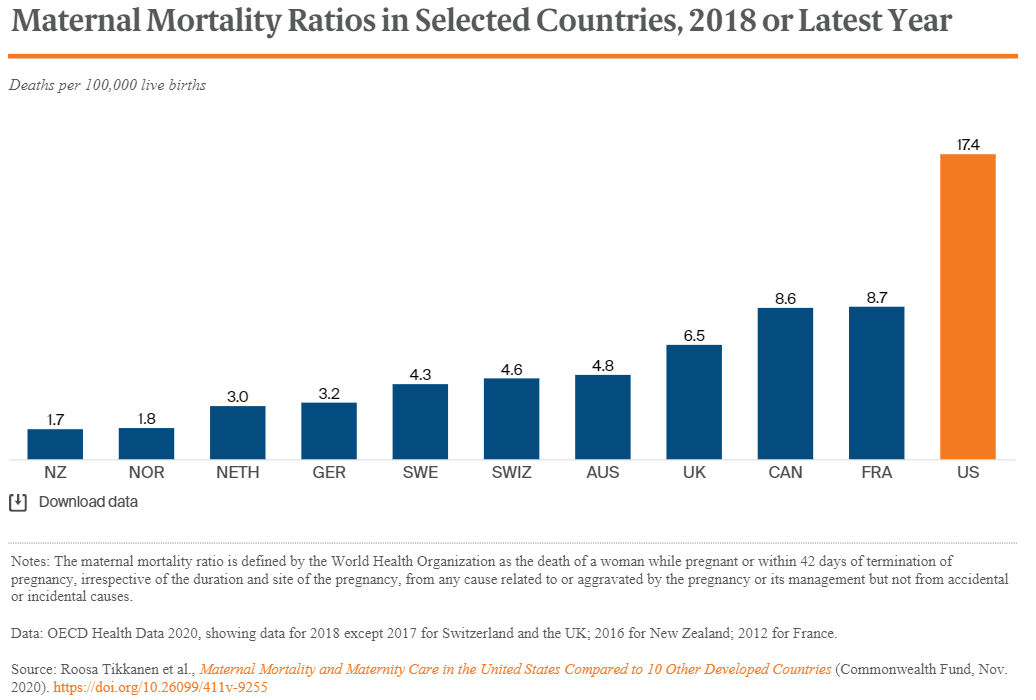
I once discussed with a nurse who had practiced in labor and delivery for many years the cesarean section rates at hospitals of up to 40%, and the fact that the United States had the worst birth outcomes in the developed world. She was offended. Nobody wants to feel like what they are doing is hurting people. We want to believe we are doing the right thing. We follow every protocol. We do everything we are trained to do. It is ingrained in us. We believe we are doing everything right.
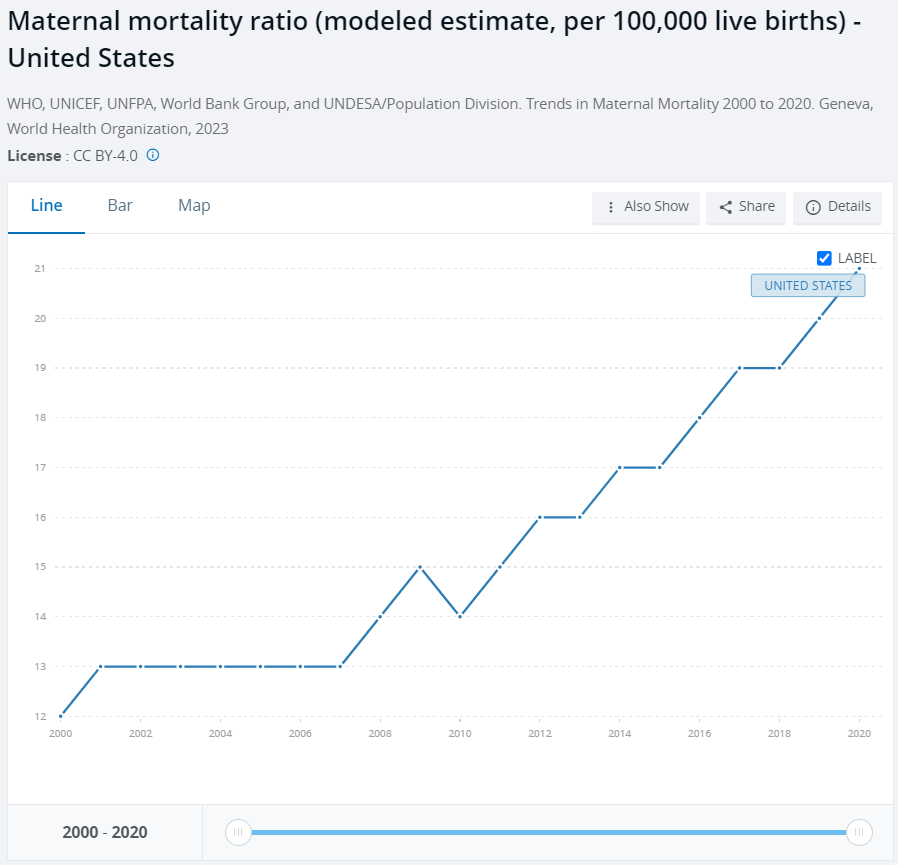
When you back up from the system, though, and look at the numbers—we are not doing everything right. Our system is killing women and children, and we are complicit in it.
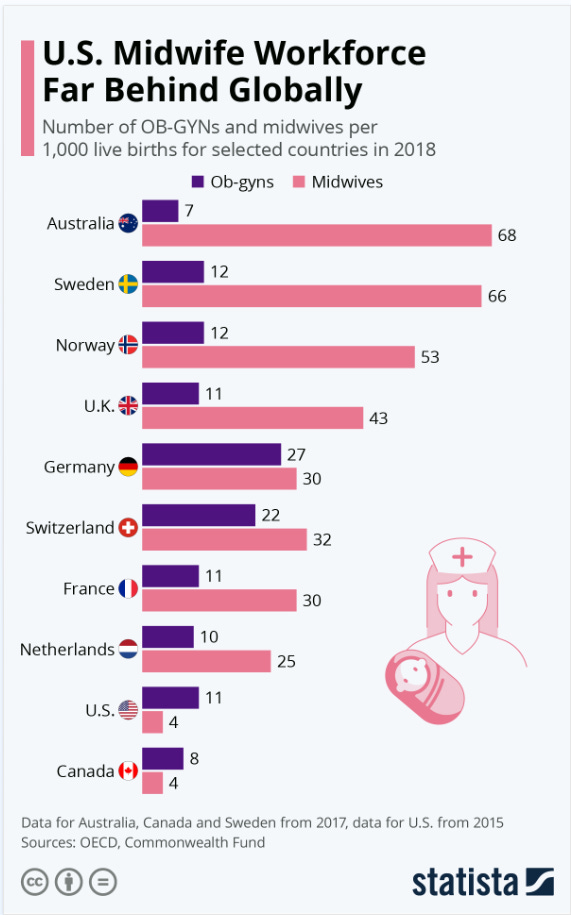
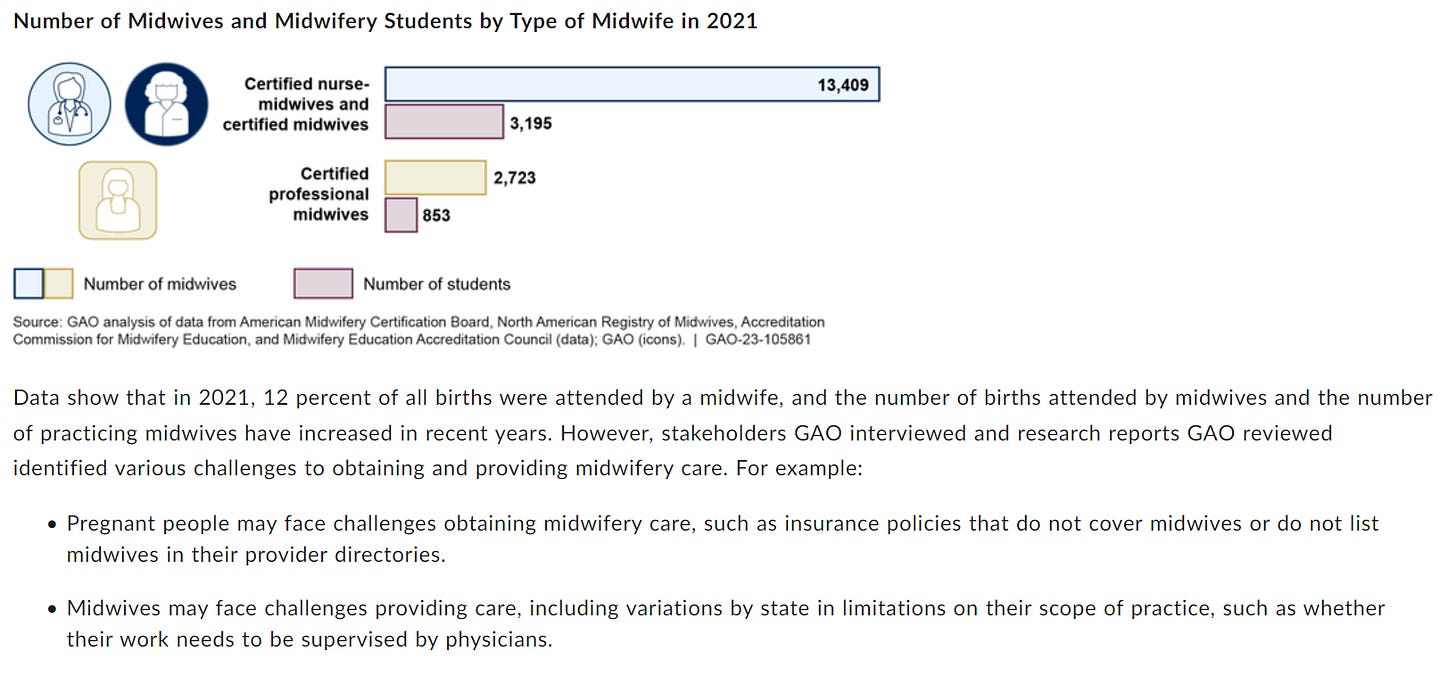
The Government Accountability Office has identified the lack of midwifery services as an area that could be improved for Maternal Mortality in the United States. I encourage you to read the whole report in the link on the picture below:
Arkansas is the only state that designates professional midwives as Licensed Lay Midwives. Everywhere else a skilled, trained, licensed midwife is designated as a Certified Professional Midwife. Most professional midwives in the state of Arkansas hold a national designation of Certified Professional Midwives. Only two of the professional midwives in Arkansas do not. To that end, for consistency, I will refer to Licensed Lay Midwives (LLM) throughout to refer to professionally licensed midwives in Arkansas (although I have learned from midwives in Arkansas that they wish the state would change the designation to Certified Professional Midwives).
If you fundamentally examine the medical model of birth, you will note that this happens in a hospital that is cold and barren, esthetically and metaphorically. It is basically a concrete box with an uncomfortable hospital bed in the middle of the room, monitors and medical equipment all around, and alarms going off everywhere. There is nothing relaxing about the space and it is not a place where people feel comfortable relaxing. The nurses, doctors, and staff are in charge here—this concept is very important. The patient or mother is a temporary, uneasy, and often unwelcome visitor in a space with nurses, doctors, and staff with all-important checklists. They are on a mission to complete their checklists, and they are hurrying to and fro. This contributes to the patient’s sense of disorientation and submission to authority. Even though hospitals talk extensively about patient-centered care, the care a woman receives in the hospital setting is very different from the care she will receive in a home environment or a birth center environment. The goal in a hospital setting is to monitor everything, restricting the patient’s movement so that the monitors will stay in place and the nurses can monitor from the nurses’ station for each anticipated intervention. What all the data tells us is that each intervention leads to more interventions and worse outcomes. This model of birth is based on fundamental fears and interventions.
A home or birth center environment is designed for the birthing woman’s comfort. It is designed to help her relax. In a home or birth center birth, all the people involved with the birth are there specifically to serve the mother. In this environment, the patient or mother is in charge and the midwives, nurses, or assistants are submissive to the needs of the mother. The goal is to give her everything she needs, whether that is music, smells, food, showers, clothing, brushing your teeth because your breath stinks, providing massage, caring for the other children, giving her something to lean on or push against and otherwise staying out of the way, and monitoring for distress or anything that would warrant a transfer to a higher level of care. This is truly patient-centered care.
Hospital births are based on fear and interventions while home or birth center births are based on allowing the birth to happen and helping the mother to relax.
In 2008 a movie came out that talked about these very issues called The Business of Being Born. I was so grateful to see a well-done piece on birth that was a better representation of what I knew home birth to be.
I am not saying there is no place for hospital births. That is not true. We need hospitals. And we need more CNMs. We most certainly need LLMs and home and birthing centers focused on helping women birth without intervening unless necessary. We need these professionals in rural areas where there are currently no birthing hospitals.
The question is really one of power and control. It is common for doctors and nurses to feel out of control when discussing home birth, Licensed Lay Midwives, or birth centers. This fear can be perceived as self-importance. However, the maternal mortality rate of LLMs in the state of Arkansas in the past 3 years is ZERO. The fear is not reflective of the statistics.
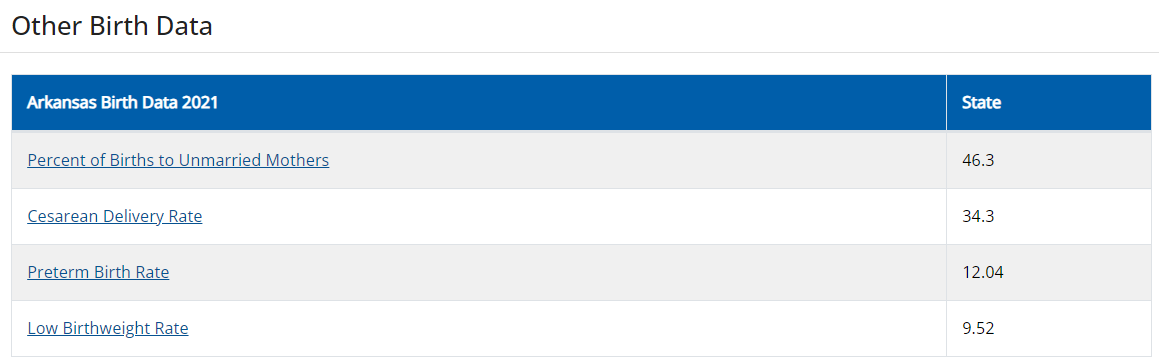
The following graph shows how the maternal mortality rate in Arkansas increased, really since 2008:
One of my heroes who died a little over a year ago was Paul Farmer. He was a medical doctor who did amazing work in communicable diseases all over the world but especially in Haiti with tuberculosis treatment. Paul brought care out into the community which is what we need to do here in Arkansas. The fact that we don’t even have birthing hospitals in most of the state is a barrier that can not be cured with the 4 mobile prenatal units that have been commissioned to provide this service. The mobile prenatal units are not birth centers staffed with CPMs. Arkansas needs to get serious about training Certified Professional Midwives in rural areas, covering their services with Medicaid, providing them with the professional support and autonomy to practice to the full extent of their licenses, as well as providing compassionate backup support for transports and collegial respect.
Unfortunately, the implementations they are currently making do not include considerations for CPMs, not that I can see anyway.
This week I am fortunate to be able to attend a couple of events about birth and reproductive health care. The first is the Northwest Arkansas Health Summit at the Fayetteville Town Center. This event has presenters from UAMS, the Arkansas Department of Health, Arkansas Advocates for Children and Families, Arkansans for Improving Maternal Health, and others. The second event is the Wellness Festival at Crystal Bridges with Olivia Walton, Tonya Lewis Lee, and Jewel. This is an interesting lineup. Olivia Walton is the wife of Walmart heir Tom Walton and she is the chair of Crystal Bridges, having replaced Alice Walton in that position. Doing an internet search on Olivia was interesting. She and her husband don’t have entries on Wikipedia and her prior journalism is difficult to find as well. Tonya Lewis Lee is the founder of Movita, a vitamin company. And Jewel is a musician who currently has an exhibit at Crystal Bridges. The line-up is all over the place so it will be interesting to see where they go with the discussion.
I’m thrilled that this topic is getting so much attention, finally. My concern is that maternal mortality in Arkansas is a multifactoral issue. Ingrained systemic race, class, and economics issues have caused these problems over hundreds of years. If we want to solve the issues we need to go into our rural areas, conduct needs assessments, have some town halls to engage with the communities, and brainstorm possibilities.
Implementing the following measures could have huge implications in Arkansas:
Getting Arkansas Medicaid to pay for CPM care
Providing incentives and funding for professional midwifery training
Providing jobs in rural communities to CPMs to help care for the births in their communities.
And improving interdisciplinary education and collegial respect between providers
I know that we should be in the rural communities having these discussions with the people who are experiencing these problems, not dictating from on high. The Certified Professional Midwives should be at the table as well as the local women in our rural communities. Right now I don’t see that happening. Maybe the events this week will prove me wrong. Maybe there are plans in the works for these implementations.
Some extra resources for my fellow birth nerds:
A country-by-country analysis of Maternal Mortality by Unicef:
Arkansas Lawmakers Consider Shifting Funds from Health Care Data Hub to UAMS Midwifery Program.
And from the Arkansas Advocate about funding the UAMS Midwifery Program.
Happy that they have included Doulas in the economic model of the hospital. It is my understanding that this is not done with Certified Professional Midwives because their practice is autonomous and not under the supervision of OB/GYNs.